Parkinson’s disease is the second most common neurodegenerative disorder worldwide, and its incidence is rapidly rising
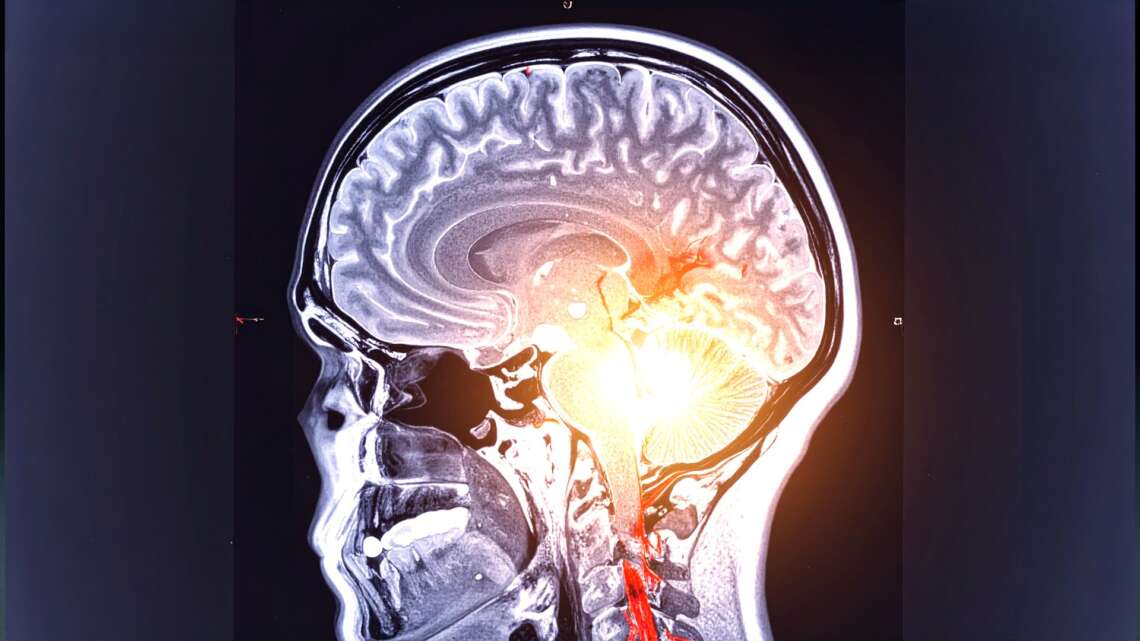
In a significant breakthrough, researchers from Simon Fraser University (SFU) in Canada have uncovered why levodopa—the mainstay drug used to treat Parkinson’s disease—does not benefit all patients equally. By using an advanced brain imaging technique known as magnetoencephalography (MEG), the team has found that the drug may sometimes activate unintended brain regions, potentially limiting its effectiveness.
The study, conducted in collaboration with the Karolinska Institute in Sweden and published in the journal Movement Disorders, maps brain signals of Parkinson’s patients before and after they take levodopa. This innovative approach has opened new avenues for developing personalised treatment strategies tailored to each patient’s brain activity profile.
Parkinson’s disease is the second most common neurodegenerative disorder worldwide, and its incidence is rapidly rising. The condition primarily affects dopamine-producing neurons in the substantia nigra region of the brain, leading to symptoms such as tremors, rigidity, slowness of movement, and balance difficulties.
Levodopa, a dopamine precursor, is the most commonly prescribed drug for alleviating these movement-related symptoms. While it works well for many, the extent of its benefit varies, with some patients experiencing only limited symptom relief. Until now, the reasons behind this variability have remained elusive.

“Treating this disease, both in terms of helping people with their symptoms and finding ways to reverse its effects, is becoming increasingly important,” said Alex Wiesman, assistant professor of biomedical physiology and kinesiology at SFU and lead author of the study. “If clinicians can see how levodopa activates certain parts of the brain in a patient, it can help to inform a more personalised approach to treatment.”
To investigate, the research team recruited 17 patients with Parkinson’s disease in Sweden and recorded their brain activity using MEG before and after administering levodopa. MEG is a highly sensitive, non-invasive imaging technology that measures magnetic fields generated by brain activity. It allows researchers to observe how medications alter neural signals in real time.
Wiesman and his team developed a novel analysis method that enabled them to “search” the brain for areas affected by the drug. What they found was surprising—levodopa occasionally activated unintended brain regions, a phenomenon described as “off-target effects.” These unexpected activations may be interfering with the drug’s therapeutic benefits.
“We found that those patients who showed off-target effects were still being helped by the drug, but not to the same extent as others,” explained Wiesman. “This finding helps explain the variability in patient responses and opens up the potential for clinicians to use MEG to optimise treatment.”
Importantly, the implications of this breakthrough go beyond Parkinson’s disease. The new brain imaging method could be applied to study the effects of any drug that targets brain signalling, potentially improving the way a wide range of neurological and psychiatric conditions are treated.
MEG is already used to study brain injuries, tumours, epilepsy, autism, and mental illnesses. Now, with this added ability to assess drug impact, it could revolutionise the field of neuropharmacology.
Wiesman hopes this research is a step toward integrating brain-based diagnostics into routine clinical care for Parkinson’s patients. By identifying how an individual’s brain responds to levodopa, doctors could better tailor medications to optimise benefits while minimising unwanted side effects.
As Parkinson’s continues to affect millions globally, such personalised treatment strategies could offer a beacon of hope for improved quality of life.